Seronegative spondyloarthropathies
![]() an acute or chronic condition
an acute or chronic condition
![]() characteristic involvement of axial joints
characteristic involvement of axial joints
![]() absence of RA factor
absence of RA factor
![]() HLA abnormality
HLA abnormality

These disorders include:
![]() Ankylosing spondylitis
Ankylosing spondylitis
![]() Reiter’s syndrome
Reiter’s syndrome
![]() Reactive arthritis
Reactive arthritis
![]() Psoriatic arthritis
Psoriatic arthritis
![]() Enteropathic arthritis-(crohn’s
disease,ulcerative colitis,whipple’s disease,behcet’s syndrome)
Enteropathic arthritis-(crohn’s
disease,ulcerative colitis,whipple’s disease,behcet’s syndrome)
![]() Juvenile-onset spondyloarthropathy
Juvenile-onset spondyloarthropathy
![]() Undifferentiated spondyloarthropathy
Undifferentiated spondyloarthropathy
Ankylosing
spondylitis
Historical
perspective:
1912 - Raymond
provided illustrations of ankylosing spondylitis in mummies and graves of
ancient
Likewise Bourke and Short described 18 instances of ankylosing
spondylitis extending over 3 millenia, 2900b.c. to 200a.d., derived from
Egyptian sources.
1850 – the modern
history of ankylosing spondylitis began with Brodie. He described a 31 year old man who had developed an
ankylosed spine and who occasionally suffered from inflammations of the eye.
1884 – Strumpell
from
1930 – the
radiographic hallmark of ankylosing spondylitis was fully recognized - sacro-iliac disease.
EPIDEMIOLOGY
Prevalence
![]() closely parallels the frequency of HLA-B27
closely parallels the frequency of HLA-B27
![]() The disease is much more common among HLA-B27-positive first-degree
relatives of (HLA-B27-positive) ankylosing spondylitis patients
The disease is much more common among HLA-B27-positive first-degree
relatives of (HLA-B27-positive) ankylosing spondylitis patients
Incidence
![]() an overall age and gender-adjusted incidence of 7.3 per 100,000
person-years
an overall age and gender-adjusted incidence of 7.3 per 100,000
person-years
![]() age of onset usually below 40 years
age of onset usually below 40 years
![]() incidence in males > incidence in females
incidence in males > incidence in females
Racial Distribution
![]() Approximately 90 percent of white patients with ankylosing
spondylitis possess HLA-B27
Approximately 90 percent of white patients with ankylosing
spondylitis possess HLA-B27
![]() Only about 50 percent of black patients with ankylosing spondylitis
possess B27
Only about 50 percent of black patients with ankylosing spondylitis
possess B27
ETIOLOGY
Hypotheses
a)
Klebsiella pneumoniae
![]()
Cross-reacting
antibodies
![]()
Bind to HLA-B27 positive
cells
![]()
Ankylosing spondylitis
b) external antigenic challenge
![]()
activation of autoreactive
t-cells
![]()
recognizes
endogenous peptides presented by HLA-B27
![]()
ankylosing spondylitis
Subtypes of
HLA-B27
Currently, 13 subtypes (allotypes) of HLA-B27 are recognized: B*2701 to
B*2713. Interestingly, 2 of the 11 subtypes--HLA-B*2706 and
HLA-B*2709--lack a strong association with ankylosing spondylitis.
Other Genetic
Factors
![]() concordance
in monozygotic twins is 63 percent, whereas concordance in all dizygotic twins
is 12.5 percent, but it rises to 23 percent in HLA-B27-positive dizygotic twins
concordance
in monozygotic twins is 63 percent, whereas concordance in all dizygotic twins
is 12.5 percent, but it rises to 23 percent in HLA-B27-positive dizygotic twins
![]() HLA-B60 has now been demonstrated to be associated with a three- to
sixfold increase in susceptibility to ankylosing spondylitis both in
HLA-B27-positive and HLA-B27-negative individuals.
HLA-B60 has now been demonstrated to be associated with a three- to
sixfold increase in susceptibility to ankylosing spondylitis both in
HLA-B27-positive and HLA-B27-negative individuals.
![]() still other HLA factors (B7-Creg, B38, B39, DR1, DR8) and non-HLA
factors (possibly Crohn's disease locus on chromosome 16 or psoriasis genes on chromosome 17) should be considered as candidates
still other HLA factors (B7-Creg, B38, B39, DR1, DR8) and non-HLA
factors (possibly Crohn's disease locus on chromosome 16 or psoriasis genes on chromosome 17) should be considered as candidates
PATHOLOGY
a)Enthesitis
![]() syndesmophyte formation, squaring of vertebral bodies, vertebral
end plate destruction, and Achilles tendonitis. Enthesitis is assosciated with
prominent edema of the adjacent bone marrow
syndesmophyte formation, squaring of vertebral bodies, vertebral
end plate destruction, and Achilles tendonitis. Enthesitis is assosciated with
prominent edema of the adjacent bone marrow
b)Sacro-iliitis
![]() Subchondral granulation tissue containing lymphocytes,plasma cells,
mast cells, macrophages and chondrocytes
Subchondral granulation tissue containing lymphocytes,plasma cells,
mast cells, macrophages and chondrocytes
![]() infiltration into ligamentous and periosteal zones
infiltration into ligamentous and periosteal zones
![]() synovitis
synovitis
![]() progression to pannus formation
progression to pannus formation
![]() The eroded and sclerotic margins of the joint are gradually
replaced by fibrocartilage regeneration and then by ossification
The eroded and sclerotic margins of the joint are gradually
replaced by fibrocartilage regeneration and then by ossification
![]() ultimately obliteration of the joint.
ultimately obliteration of the joint.
c)Spine
![]() Early
inflammatory granulation tissue at the junction of the annulus fibrosus of the
disk cartilage and the margin if the vertebral bone
Early
inflammatory granulation tissue at the junction of the annulus fibrosus of the
disk cartilage and the margin if the vertebral bone
![]() erosion
of the outer annular fibers->replaced by bone
erosion
of the outer annular fibers->replaced by bone
![]() forming
a bony excrescence called syndesmophyte->continues to grow by enchondral
ossification
forming
a bony excrescence called syndesmophyte->continues to grow by enchondral
ossification
![]() bridging
the adjacent vertebral bodies->ascending progression of this process leads
to bamboo spine
bridging
the adjacent vertebral bodies->ascending progression of this process leads
to bamboo spine
![]() Inflammatory arthritis of the apophyseal joints->erosion of the
cartilage by pannus->bony ankylosis.
Inflammatory arthritis of the apophyseal joints->erosion of the
cartilage by pannus->bony ankylosis.

![]() Bone mineral density is diminished in the spine and the proximal
femur early in the course of the disease
Bone mineral density is diminished in the spine and the proximal
femur early in the course of the disease
d)Eyes
e) Aortic valve
![]() Aortic insufficiency
Aortic insufficiency
![]() A-V blocks
A-V blocks
f) Others
![]() Colonic lesions
Colonic lesions
![]() IgA nephropathy
IgA nephropathy
CLINICAL MANIFESTATIONS
Skeletal Manifestations
![]() Low Back Pain and Stiffness
Low Back Pain and Stiffness
![]() Chest Pain
Chest Pain
![]() Tenderness
Tenderness
![]() Joints
Joints
Extraskeletal Manifestations
![]() General Symptoms
General Symptoms
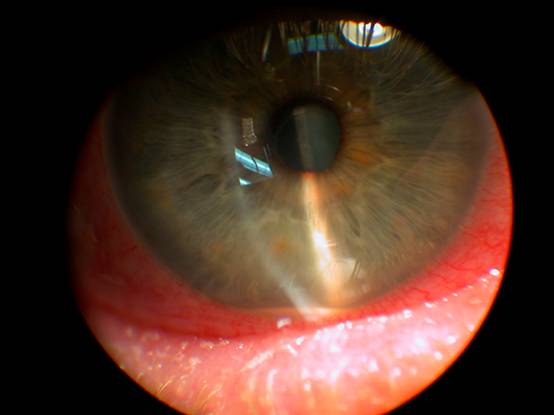
![]() Eye Disease
Eye Disease
![]() Cardiovascular Disease
Cardiovascular Disease
![]() Pulmonary Disease
Pulmonary Disease
![]() slowly progressive fibrosis of the upper lobes
of the lungs
slowly progressive fibrosis of the upper lobes
of the lungs
The lesions eventually become cystic
![]()
the cavities may subsequently be colonized by Aspergillus, with
the formation of mycetoma (cough, hemoptysis, dyspnea)

![]() Neurologic Involvement:-
Traffic accidents or minor trauma can cause spinal
fractures. The C5-C6 or C6-C7 level is the most commonly involved site, atlantoaxial
joint subluxation, atlanto-occipital subluxation, and upward subluxation of the
axis may occur in ankylosing spondylitis as a consequence of instability
resulting from the inflammatory process.
Causes of neurologic complications due to
compression include ossification of the posterior longitudinal ligament (which
may lead to compressive myelopathy), destructive intervertebral disk lesions,
and spinal stenosis. The cauda equina syndrome is a rare but serious complication of
long-standing ankylosing spondylitis.
Neurologic Involvement:-
Traffic accidents or minor trauma can cause spinal
fractures. The C5-C6 or C6-C7 level is the most commonly involved site, atlantoaxial
joint subluxation, atlanto-occipital subluxation, and upward subluxation of the
axis may occur in ankylosing spondylitis as a consequence of instability
resulting from the inflammatory process.
Causes of neurologic complications due to
compression include ossification of the posterior longitudinal ligament (which
may lead to compressive myelopathy), destructive intervertebral disk lesions,
and spinal stenosis. The cauda equina syndrome is a rare but serious complication of
long-standing ankylosing spondylitis.
![]() Renal
Involvement
Renal
Involvement
![]() Osteoporosis
Osteoporosis
PHYSICAL FINDINGS
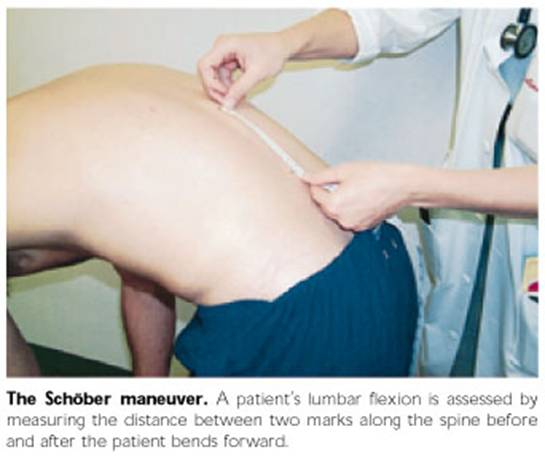
![]() Spinal Mobility:- there is usually some limitation of motion of
the lumbar spine as elicited by forward flexion, hyperextension, or lateral
flexion. Early loss of the normal lumbar lordosis is easily assessed on
inspection.
Spinal Mobility:- there is usually some limitation of motion of
the lumbar spine as elicited by forward flexion, hyperextension, or lateral
flexion. Early loss of the normal lumbar lordosis is easily assessed on
inspection.
![]() Chest Expansion
Chest Expansion
![]() Enthesitis
Enthesitis
![]() Sacroiliitis
Sacroiliitis
![]() Posture
Posture
LABORATORY FINDINGS
![]() elevated
erythrocyte sedimentation rate
elevated
erythrocyte sedimentation rate
![]() elevated level
of C-reactive protein
elevated level
of C-reactive protein
![]() mild
normochromic, normocytic anemia
mild
normochromic, normocytic anemia
![]() elevated
alkaline phosphatase level
elevated
alkaline phosphatase level
![]() Elevated serum
IgA levels
Elevated serum
IgA levels
![]() Rheumatoid
factor and antinuclear antibodies are largely absent unless caused by a
coexistent disease.
Rheumatoid
factor and antinuclear antibodies are largely absent unless caused by a
coexistent disease.
![]() Synovial fluid
from inflamed peripheral joints in AS is not distinctly different from that of
other inflammatory joint diseases
Synovial fluid
from inflamed peripheral joints in AS is not distinctly different from that of
other inflammatory joint diseases
![]() In cases with
restriction of chest wall motion, decreased vital capacity and increased
functional residual capacity are common, but airflow measurements are normal
and ventilatory function is usually well maintained
In cases with
restriction of chest wall motion, decreased vital capacity and increased
functional residual capacity are common, but airflow measurements are normal
and ventilatory function is usually well maintained
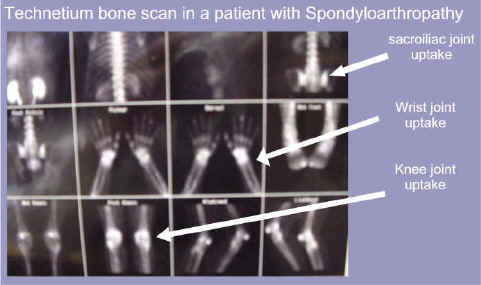
RADIOGRAPHIC FINDINGS
Roentgenographic
abnormalities generally appear in the sacroiliac joints before appearing
elsewhere in the spine. Radiographically demonstrable sacroiliitis is usually present
|
Grading of Sacroiliitis According to theNew
York Criteria |
|
Grade |
|
0, |
|
1, Suspicious |
|
2, Minimal sacroiliitis |
|
3, Moderate sacroiliitis |
|
4, Ankylosis |

demonstrates ankylosis of the sacroiliac
joints

dynamic MR
imaging with a T1 -weighted sequence after intravenous injection of
gadolinium diethylenetriaminepentaacetic acid (Gd-DTPA) might be considered to
demonstrate early stages of sacroiliitis

Early sacroiliitis
of ankylosing spondylitis. acute sacroiliitis the right side, with edema in the
juxtaarticular bone marrow (asterisks), in the region of the synovium
and joint capsule (thin arrow), and in the region of the interosseous
ligaments (thick arrow). Early chronic changes, including cortical
erosions and joint space widening, were evident in the right sacroiliac joint
DIAGNOSIS
|
Criteria |
|
1. Low back
pain at least 3 months' duration improved by exercise and not relieved by
rest |
|
2.
Limitation of lumbar spine in sagittal and frontal planes |
|
3. Chest
expansion decreased relative to normal values for age and sex |
|
4.
Bilateral sacroiliitis grade 2-4 |
|
5.
Unilateral sacroiliitis grade 3-4 |
|
Definite
ankylosing spondylitis if unilateral grade 3 or 4, or bilateral grade 2-4
sacroiliitis and any clinical criterion |
PROGNOSIS
The course of
ankylosing spondylitis is highly variable. Characterized by spontaneous
remissions and exacerbations, it is generally favorable because the disease is
often relatively mild or self-limited.
TREATMENT
![]() Exercises
Exercises
![]() Ergonomics
Ergonomics
![]() Physiotherapy
Physiotherapy
![]() Indomethacin is particularly effective as a 75-mg slow-release
preparation taken once or twice daily
Indomethacin is particularly effective as a 75-mg slow-release
preparation taken once or twice daily
![]() phenylbutazone, at doses of 200 to 400 mg/d, has been considered
the most effective anti-inflammatory agent in AS
phenylbutazone, at doses of 200 to 400 mg/d, has been considered
the most effective anti-inflammatory agent in AS
![]() sulfasalazine, in doses of 2 to 3 g/d, is useful in reducing
peripheral joint symptoms as well as reversing laboratory evidence of
inflammation
sulfasalazine, in doses of 2 to 3 g/d, is useful in reducing
peripheral joint symptoms as well as reversing laboratory evidence of
inflammation
![]() The peripheral arthritis may also respond to the folic acid
antagonist methotrexate
The peripheral arthritis may also respond to the folic acid
antagonist methotrexate
![]() Occasionally, intralesional or intraarticular glucocorticoid injections
may be beneficial in patients with persistent enthesopathy or synovitis
unresponsive to anti-inflammatory agents
Occasionally, intralesional or intraarticular glucocorticoid injections
may be beneficial in patients with persistent enthesopathy or synovitis
unresponsive to anti-inflammatory agents
![]() anti–TNF-α agents: etanercept
anti–TNF-α agents: etanercept
![]() Attacks of iritis are usually effectively managed with local
glucocorticoid administration in conjunction with mydriatic agents, although
systemic glucocorticoids or even immunosuppressive drugs may be required in
some cases
Attacks of iritis are usually effectively managed with local
glucocorticoid administration in conjunction with mydriatic agents, although
systemic glucocorticoids or even immunosuppressive drugs may be required in
some cases
![]() Coexistent cardiac disease may require pacemaker implantation
and/or aortic valve replacement.
Coexistent cardiac disease may require pacemaker implantation
and/or aortic valve replacement.
![]() The most common indication for surgery
in patients with AS is severe hip joint arthritis, the pain and
stiffness of which are usually dramatically relieved by total hip arthroplasty.
Vertebral osteotomy may be required in selected cases to correct marked flexion
deformity
The most common indication for surgery
in patients with AS is severe hip joint arthritis, the pain and
stiffness of which are usually dramatically relieved by total hip arthroplasty.
Vertebral osteotomy may be required in selected cases to correct marked flexion
deformity